Degenerative Disc Disease is often misunderstood. It is not a disease per se, but rather a painful reaction to normal changes in the spine.
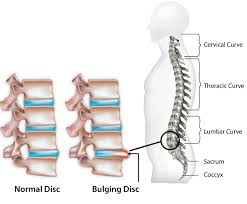
The spine is made up of small bones called vertebrae. The vertebrae are stacked on top of each other with cushy discs in between. These spinal discs are complex structures composed of cartilage on the outside and a gelatinous core on the inside. The best way to think of them is like a jelly donut.
When we are young spinal discs are larger and more squishy (that’s the technical term). They support our vertebrae and allow our spines to be flexible. As we age, these discs shrink and harden. This results in less tolerance to absorb shock and less flexibility. Nearly everyone feels this change in flexibility as they age, but not everyone experiences back pain as a part of aging.
Disk degeneration is a catchall phrase for several different types of age-related changes that can happen in the spine. These include flattening and hardening of the disc- sometimes referred to as arthritis of the spine, cracked or herniated discs, and bulging discs. When any of these changes cause pain, you have Degenerative Disc Disease. Each of these changes can have unique symptoms and different prognoses.

Who Experiences Degenerative Disc Disease
Degenerative Disc Disease is caused by normal wear and tear. About 30% of people have some disc degeneration by the age of 35. By age 60, more than 90% of people have degenerated discs. It is not a “disease” unless it is causing you pain. Back pain associated with disc degeneration is relatively common in people over the age of 30.
What are the Symptoms
As stated above, symptoms can vary depending on the type of degeneration that is taking place:
Arthritis
If you have discs that have thinned and broken down, you may be told you have arthritis in your spine. Just like arthritis in other joints, spinal arthritis refers to a condition where the cartilage- in this case, the discs- are no longer providing proper cushioning and lubrication for the joint. As a result, the vertebrae might rub together.
Many people have some arthritis in their spine, and most never experience pain. If your vertebrae form bones spurs–bony projections along the edges of a bone- in reaction to the arthritis, your risk of experiencing pain increases. Sometimes these spurs can interfere with your spinal cord causing pain and numbness or tingling in the extremities.
Even some people with bone spurs never experience pain, but if you have arthritis in your spine, you will probably notice stiffness and reduced flexibility. Osteoarthritis of the spine most commonly occurs in the lower back or the neck. The most common symptoms are pain and stiffness. The pain can range from mild to severe and will feel better when you lay down and worsen with standing or walking. It may come and go, flaring up at certain times and dying down at others. Or you may experience some level of pain every day.
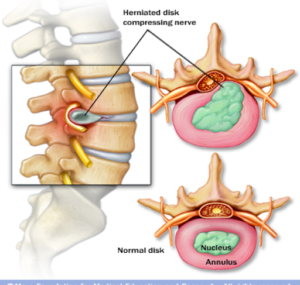
Herniated Disc
If a torn disc is causing your pain, it may be more acute and severe than the pain caused by arthritis. Small tears in the outer cartilage of spinal discs are common and usually don’t cause discomfort. Sometimes a tear is large enough that the inner gelatinous part of the disc pushes through the tear. This is called a herniated disc. The gelatinous substance inside the disc contains proteins that cause inflammation and irritation to nerves and tissue that it touches. When it leaks out of the disc, it can cause pain to come on suddenly. Sometimes the pain is mild, but it can also be severe.
Unlike the ache associated with arthritis, pain from a torn disc is usually described as burning or sharp. If the herniated disc occurs in your back, you may feel pain in your thighs and buttocks. If it occurs in your neck, the pain may radiate through your shoulder and arm. In rare severe cases, a herniated disc can irritate the nerves that deal with bladder and bowel control. If you experience a loss of bladder or bowel control, you should go to the emergency room immediately.
Numbness, tingling, and weakness in the limbs affected by the disc is a common side effect and usually not cause for alarm. You may find that the pain shoots through your arm or leg when you move a certain way or when you cough or sneeze. Pain from a herniated disc will feel better when you are walking around and worse when you are standing still or sitting.
Bulging Discs
A bulging disc is a disc that is bulging abnormally out from between the vertebrae. Often this will have no symptoms, but if it puts pressure on a pressure point, you may experience strange sensations like numbness and tingling in the extremities. If the bulging disc is in the neck, these sensations will be felt in the arms and hands. If it is in the lower back, you will feel them in your legs. A bulging disc impacting the sciatic nerve will cause pain to shoot down only one thigh. Bulging discs often become herniated discs.

How Do I Feel Better?
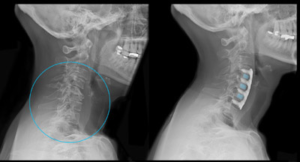
Treatment will also depend on what type of degeneration you are experiencing. Usually, arthritis and herniated discs can be managed at home and with the help of a chiropractor or physical therapist. If the pain and nerve symptoms are severe and long-lasting, you may need to have x- rays or a CT scan to pinpoint the problem and come up with a specific treatment plan. A range of therapies, including hot/cold therapy, massage, physical therapy, and spinal decompression, can be used to reduce pain and increase mobility.
98% of herniated discs resolve without surgery, usually within four to six weeks. Surgery is only prescribed for spinal arthritis if bone spurs are interfering with the spinal cord or if the pain has not responded to other treatments and is interfering with everyday life.
If your pain is only flaring up occasionally, you can treat it with over the counter pain relievers or massage. Physical therapy may also be helpful and can teach you exercises that you can do on your own to prevent pain. Losing weight and quitting smoking may also help.
If you suffer from chronic or severe pain, spinal decompression therapy may help your body heal. Spinal decompression involves gentle traction that stretches the spine, creating negative pressure between the vertebrae. This helps to retract bulging or herniated discs and increases the movement of oxygen, water, and nutrient-rich fluids around the disc, promoting healing. The treatment also takes the pressure off of nerves.
Spinal decompression is a comfortable, non-invasive procedure that has been shown to reduce pain permanently. After a series of treatments, patients can see a 70% reduction in their back pain. Spinal decompression can reduce your need for NSAIDs and other pain killers that may have harmful side effects.